Full Guide for doctors on how AI scribes change clinical documentation, reduce admin work, and help clinics finish SOAP notes faster in 2026.
Clinical documentation has always been a weird paradox. It’s one of the most important parts of patient care, and also one of the most exhausting parts of patient care. Notes protect patients, support continuity, satisfy billing and compliance, and communicate clinical thinking. But they also eat time, create after-hours charting, and quietly drive burnout. Over the last few years, something has shifted. AI scribes moved from “interesting experiment” to “daily workflow tool,” and the change is accelerating.
In 2026, the conversation isn’t whether AI scribes work. It’s how they fit into real-world clinic operations, what “good” looks like, and how clinicians can adopt them without creating more friction. If you run a private practice, work in an outpatient clinic, or see patients back-to-back in a hospital setting, this matters. AI scribes aren’t just faster typing. They’re changing the shape of clinical work.
For most clinicians, documentation pain is not about speed alone. It’s about context switching. You listen, you assess, you think, you reassure, you decide, then you flip into “clerical mode” and try to reconstruct everything precisely. When the day is packed, those transitions pile up. You end up with notes that are either delayed, incomplete, or rushed. Even if you’re fast, the workload doesn’t feel light because your brain is constantly jumping between patient care and administrative capture.
Traditional solutions tried to patch the workflow. Templates became longer. Copy-forward became common. Macros and dot phrases got better. Some clinics hired scribes, which helped, but came with training, cost, turnover, and the reality that not every specialty or budget can support it. The core issue remained: documentation happens after the clinical moment, and that gap creates risk and stress.
The biggest change AI scribes bring is timing. Instead of reconstructing the visit later, clinicians can capture the encounter while it’s fresh, either during the visit or immediately after. That alone is a major shift because the “memory tax” disappears. You’re no longer trying to remember exactly which symptoms were denied, what the patient said about onset, or the nuance of shared decision-making. When documentation moves closer to the moment, notes become more accurate, more complete, and less emotionally draining.
This is why AI scribes are impacting more than productivity. They’re affecting quality. The note becomes a reflection of what truly happened, not what you can recall at 8:30 PM after the last patient.
Early “AI scribe” tools were basically transcription apps dressed up for healthcare. They captured audio, produced a text dump, and then asked clinicians to clean it up. That’s not a scribe. That’s another inbox.
What’s changing now is structure. The newest generation of AI scribes is designed to turn conversations into clinically useful formats. SOAP notes, H&P, progress notes, procedure notes, referral letters, patient instructions, prior authorization summaries, and specialty-specific templates are becoming the baseline expectation. Clinicians don’t want more text. They want the right note, in the right format, ready to review.
This is also where adoption is growing fastest. When a tool saves 10–20 minutes but still leaves you with a messy output, clinicians tolerate it briefly and then abandon it. When a tool saves time and produces something you’d actually sign, it becomes part of the routine.
One of the most meaningful workflow shifts is that clinicians are spending less time drafting and more time reviewing. That’s a healthier role. Clinicians should be validating clinical reasoning, ensuring accuracy, and confirming key details. They shouldn’t be spending their best mental energy on formatting, phrasing, and repetitive sections.
AI scribes are turning documentation into something closer to radiology reporting workflow: you review, you edit what matters, you sign. This subtle shift reduces cognitive load and makes documentation feel less like a second job.

A lot of marketing around AI scribes focuses on “time saved.” That’s true, but the deeper impact is clinic flow. When documentation becomes lighter, small operational improvements appear everywhere.
Visits run less behind because the clinician isn’t mentally tracking “things I need to write later.” Handoffs improve because notes are completed earlier. Patient messaging becomes faster because the encounter record is clearer. Coding support becomes easier because the documentation contains the clinical story and decision-making. The end of day feels less like an unfinished pile of obligations.
For private practices, this also touches revenue indirectly. Faster note completion can mean cleaner billing processes, fewer rejected claims due to missing documentation elements, and less need for post-visit chart chasing. For hospital-based outpatient clinics, it can improve throughput and reduce the documentation backlog that causes weekend catch-up work.
In 2026, “general note generation” is no longer enough. Specialties document differently. A dermatologist’s note structure, a psychiatrist’s clinical narrative, an orthopedic exam, an OB/GYN visit, and a cardiology follow-up are not interchangeable. The AI that wins is the one that respects specialty nuance while still being fast.
Clinicians are also asking for more control. Not everyone wants the same style. Some want a very concise assessment and plan. Some want more narrative for complex patients. Some need specific billing-friendly sections like MDM, ROS, and exam elements. Others prioritize patient-friendly instructions that can be copied into after-visit summaries.
This is why customizable templates matter. A tool that can adapt to your style rather than forcing you into one format will always have higher retention. The “one-size-fits-all” era is fading.
The obvious concern with AI scribes is privacy and control. Clinics want to know what’s being recorded, where it’s stored, how it’s processed, and who can access it. But there’s also a practical concern that matters just as much: relevance. Capturing everything is not the goal. Capturing what’s clinically meaningful is the goal.
Modern AI scribes are evolving to focus on clinically relevant content, reduce filler, and support workflows where the clinician can confirm key sections quickly. The best tools support review, redaction where necessary, and consistent formatting so notes don’t look like a raw transcript.
This isn’t just compliance talk. It’s adoption reality. Clinicians need to feel in control of their documentation output, and patients need to feel respected during the visit.
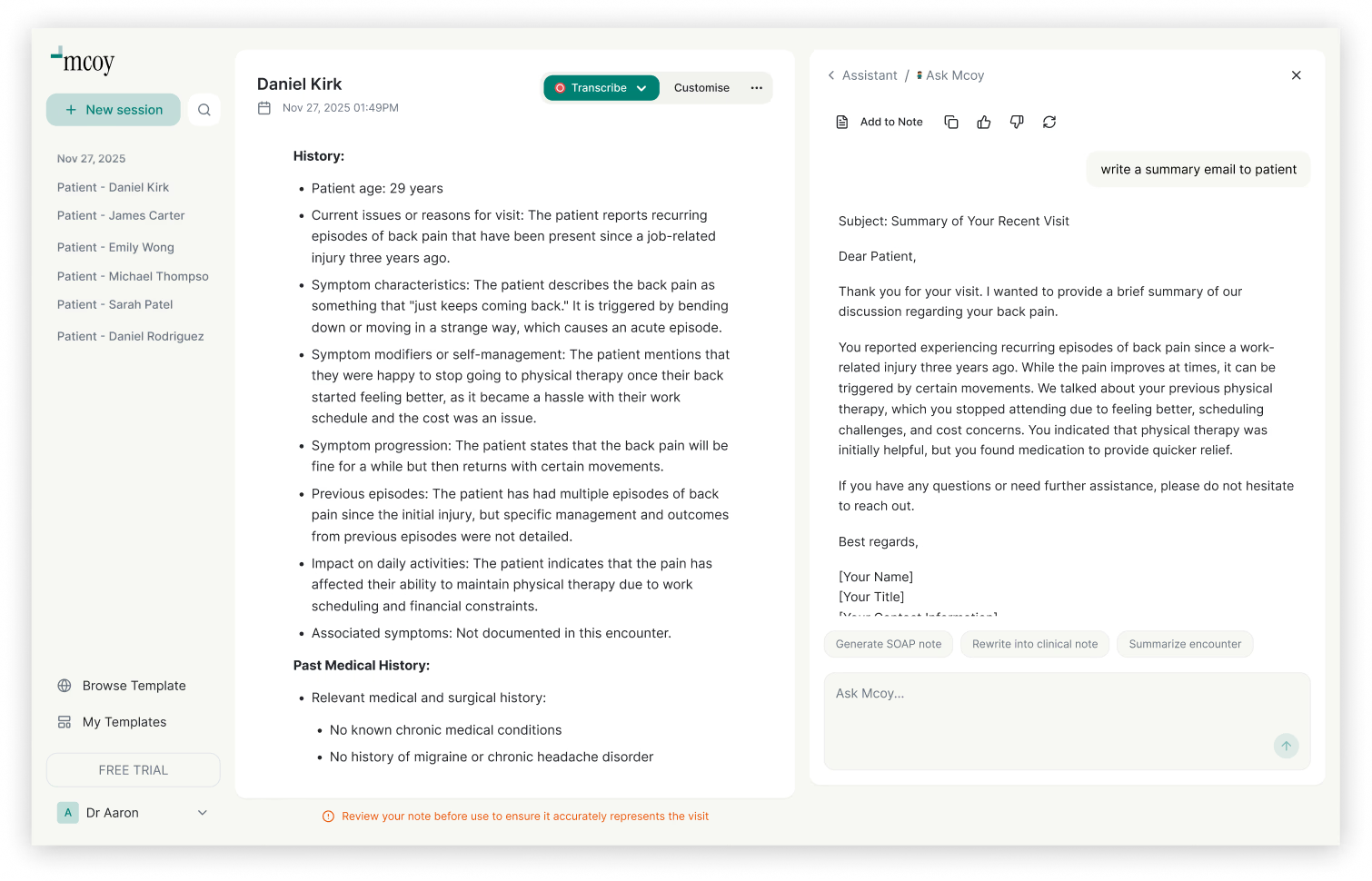
Mcoy AI is built for the reality of busy clinic days where documentation piles up fast. It can record and transcribe patient encounters, then turn them into structured clinical notes like SOAP, with over 200+ customizable templates designed for different specialties and workflows. Beyond notes, Mcoy AI lets clinicians chat with their encounters to quickly pull key details, and generate documents like forms and letters using ChatGPT built in, so you can reduce admin work and focus more on care.
What makes this useful in practice is that it supports how clinicians actually work. You don’t need another tool that produces a wall of text. You need something that gives you a note you can sign, in the format you prefer, and the flexibility to create supporting documentation without reopening the encounter in your head from scratch.
AI scribes will keep evolving, but the direction is already clear. Documentation becomes more immediate, more structured, and more connected to downstream admin tasks. The best systems will behave less like “an app you open” and more like “a workflow layer” that follows the patient encounter from conversation to note to billing-ready documentation to follow-up materials.
Clinicians will increasingly expect three things.
First, consistent output quality. Notes should be usable, not just impressive demos.
Second, specialty alignment. The tool must respect how your specialty documents and codes.
Third, administrative extension. After the note, you should be able to generate the supporting items that steal time: letters, forms, referral summaries, patient instructions, and structured documentation for payers.
If you’re considering adding an AI scribe to your practice or clinic workflow, the smoothest adoption is simple.
Start with a narrow use case, like follow-up visits or one clinic session per week, and measure whether notes are faster to finalize. Use a consistent template so your team sees predictable structure. Build a quick review habit, focusing on accuracy in HPI, assessment, meds, and plan. Once you trust the output, expand gradually.
It’s also worth aligning with your clinic’s priorities. If your biggest pain is after-hours charting, optimize for note completion speed. If your biggest pain is inconsistent documentation for billing, optimize for structure and MDM clarity. If your biggest pain is admin paperwork, prioritize tools that generate letters and forms from the encounter context.
AI scribes are changing documentation from a burden into a manageable review step. That doesn’t mean clinicians stop thinking or stop being responsible for the note. It means the worst parts of documentation, the repetitive capture, formatting, and reconstruction, can fade into the background. As this becomes normal, the competitive advantage for clinics won’t be who types faster. It will be who runs smoother, finishes notes faster, and protects clinician energy while maintaining high-quality documentation.
For busy clinics and private practitioners, that shift isn’t just convenient. It’s a structural upgrade to how care gets delivered.
FAQ
They can be, but accuracy depends on workflow and review. The safest approach is to treat AI output as a draft you verify, especially around medications, allergies, numbers, and the assessment and plan. Over time, once you trust the tool and your templates, review becomes faster.
In many clinics they reduce the need for human scribing, but the best comparison is that they replace the repetitive capture and formatting work. Some teams still use staff for coordination and chart prep, while AI handles the note drafting.
It can improve it if used thoughtfully. When documentation burden is reduced, clinicians can maintain more eye contact and focus. It’s important to be transparent about recording and make sure the workflow doesn’t feel intrusive.
Look for structured clinical outputs, specialty templates, customization, fast review flow, and the ability to generate supporting documents like letters and forms from the same encounter context.
Many clinics start within days by testing on a subset of visits. The key is to standardize templates, set review habits, and expand gradually once output quality is consistent.